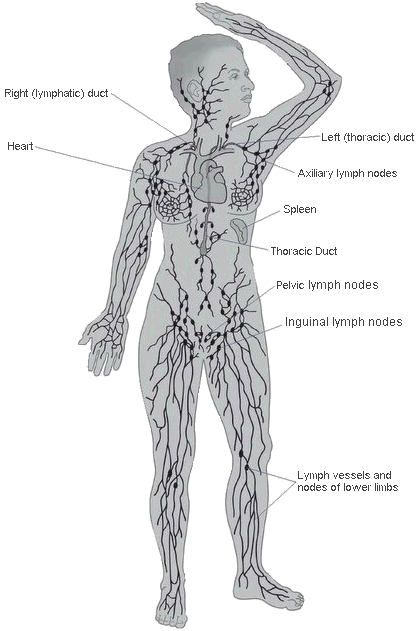
| WHAT IS LYMPHEDEMA? Lymphedema is chronic swelling (edema) caused by a buildup of fluid (lymph). This happens when the lymphatic system is either faulty or damaged and cannot function as normal. It leads to chronic (long-lasting) swelling in the tissues where the lymph flow is blocked. Lymphedema most commonly presents in a limb (arm/hand or leg/foot), but it can also be present in the breast, trunk, genitals, or head and neck.
USEFUL LINKS TO LEARN MORE ABOUT THE LYMPHATIC SYSTEM The Lymphatic System https://www.cdc.gov/cancer/survivors/patients/lymphedema.htm http://www.vodderschool.com/lymph_vessel_system
It is estimated that 1 million Canadians have the incurable disorder, many unaware of the true cause of their swelling which is often misinterpreted as fat. There are many causes of lymphedema classified into two forms: Primary lymphedema is caused by a defect of the lymphatic system. It may be present at birth, develop when puberty begins or in adulthood.
Secondary lymphedema is caused due to an event that damages or blocks part of the lymphatic system. The most common cause is the result of treatment for some cancers (surgery, radiation). Other causes of damage to the lymphatic system include trauma caused by an accident, injury or a burn. · Abnormal swelling in the affected body part · Full or heavy feeling in the affected body part · Decreased mobility or achy in the affected body part · Clothing, jewellery or shoes may feel tighter but not due to weight gain
If you feel unwell or notice a sign of infection such as increased redness, swelling, warmth or pain to the affected limb, you should be seen by your doctor or emergency personnel immediately. At present there is no cure for lymphedema; however, it can be successfully managed if diagnosed and treated in a timely manner. Stages help classify the severity of Lymphedema. Currently there are four (4) known stages ranging from mild to severe. Stage 0 (latent) – The least severe of all and not truly visible. Stage 1 (early or mild) – Lymphedema is reversible as the swelling will disappear with elevation or bedrest. Stage 2 (moderate) – Elevating does not resolve swelling. Stage 3 (severe) – Most advanced stage. Your risk for lymphedema depends on a number of factors, including: ● A family history of chronic (long-lasting) swelling ● If you had surgery, the number, size and location of lymph nodes removed or damaged ● If you had radiation therapy or an injury, the degree of damage to your lymphatic system ● Having chronic venous disease ● Having a history of skin infections, including cellulitis ● Being overweight and/or inactive add to these risk factors Having a risk factor doesn’t mean you’re going to develop lymphedema but if your lymphatic system is faulty or damaged, you have a lifetime risk for lymphedema. We can’t predict who’s going to develop lymphedema. Your body may heal well after treatment and be able to manage the lymph flow in the damaged area. Or, the extent of damage to your lymphatic system may combine with other risk factors and trigger lymphedema during treatment or many years later. Risk Reduction strategies when living with lymphedema:
You may find it helpful to speak to a certified lymphedema therapist about your risk for lymphedema and ways to lower it. This information does not replace the advice of a qualified health care professional. | ||
|

.png)
 The
The